Spine • Joint • Nerve • Mild Traumatic Brain Injury
Board-Certified Surgeons & Fellowship-Trained Pain Specialists | Hablamos Español
Go to the ER/Call 911 for severe/worsening headache after head impact, loss of consciousness, new bowel/bladder changes, rapidly progressing weakness, chest pain, or breathing difficulty.

Focused history & exam tailored to your mechanism of injury
Right-sized plan: activity guidance, bracing, home measures, medications when appropriate
Fluoroscopy-guided injections for select spine/joint pain generators when indicated
Imaging coordination (MRI/CT/X-ray) only if results would change management
Rehab roadmap with milestone-based return to work/sport
Objective documentation of findings, treatments, and functional progress
Typical issues: Whiplash/cervical strain, low-back pain and disc herniation, shoulder/knee impact injuries, headaches and nerve irritation
Our approach: Targeted exam, function-first plan, fluoro-guided procedures when appropriate, and coordinated MRI/CT only if results guide care. Rehab progression focuses on mobility, strength, and safe return to driving/work.

Typical issues: Lumbar strain/facet irritation, shoulder tendinopathy, carpal tunnel, knee/ankle sprains.
Our approach: Mechanism-based restrictions, stepwise pain control, fluoro-guided options when indicated, return-to-work progression with clear capacity notes.

Typical issues: ACL/MCL/meniscus, labrum/rotator cuff, high ankle sprains, stress reactions, post-impact headaches/concussion symptoms.
Our approach: Sport-specific assessment, graded loading, bracing/taping guidance, fluoro-guided procedures when appropriate, imaging for surgical vs non-surgical decisions, milestone-based return-to-play.

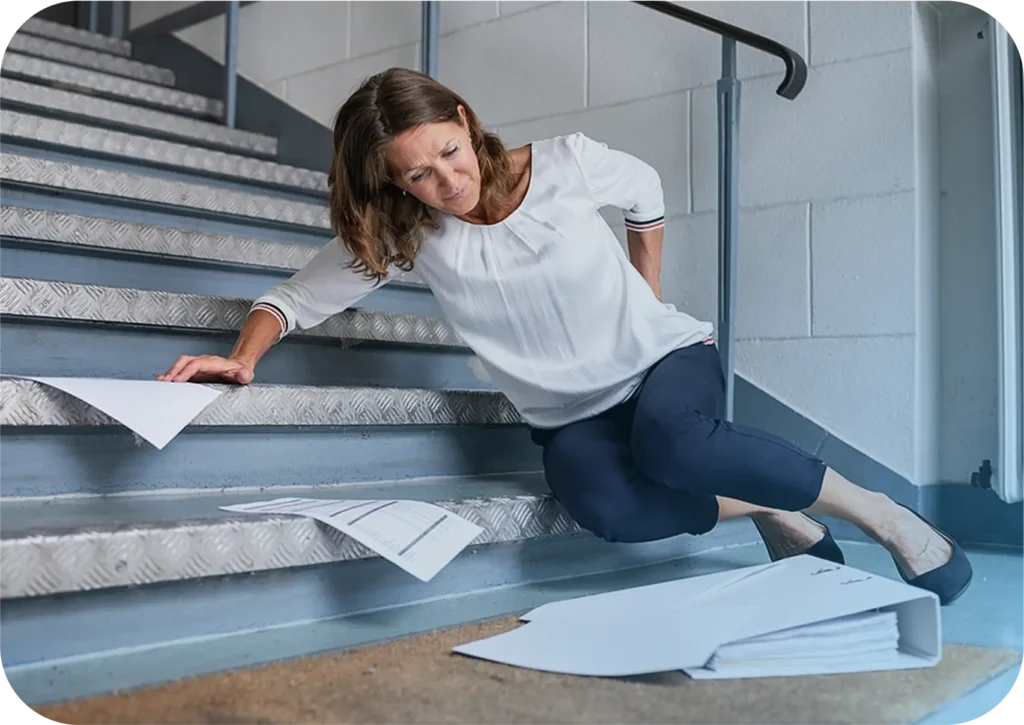
Typical issues: Wrist/hip fractures, ankle/knee ligament injuries, spinal compression fractures, dizziness or concussion symptoms, gait changes.
Our approach: Safety-first assessment, stabilization, fluoro-guided pain procedures when indicated, imaging coordination for suspected fracture/ligament injury, plus balance & strength rehab to reduce future falls.

Our step-by-step approach provides progressive care, starting with the least invasive options and advancing only when necessary.
Any prior MRI/CT/X-rays and reports
(if available)
Medication list, allergies, brief
timeline of injury and symptoms
Your job/sport demands to tailor
restrictions and progression
Braces/orthotics you currently use;
wear comfortable clothing for
movement testing

Board-Certified Orthopedic Surgeon

Board-Certified Radiologist & Neuroradiologist

Board-Certified Pain Management & Rehabilitation Specialist
Request Your Same-Day Injury & Trauma Care Evaluation
Don’t wait in pain — our expert spine specialists are available for same-day evaluations.
Not usually. We start with a focused history and exam to determine if imaging would change your care. When imaging is indicated, we coordinate MRI, CT, or X-ray through trusted independent centers. Many injuries improve with a structured plan without immediate scans. If red-flag symptoms arise, we expedite imaging and referral to ensure management tailored to your needs.
Conservative care first: activity modification, home measures, medications, and rehabilitation. If pain generators persist and improvement stalls, we may consider fluoroscopy-guided injections for relief and diagnostic clarity. Surgery is reserved for indications like instability, neurologic deficit, or structural problems unlikely to resolve conservatively. Decisions are individualized, evidence-informed, and focused on restoring function and returning you to daily life.
Call us. We often have urgent openings. We’ll triage symptoms, offer guidance before your visit, and schedule promptly today. If you have red-flag symptoms—worsening weakness, bowel or bladder changes, severe head injury, chest pain, or trouble breathing—seek emergency care right away. Otherwise, early evaluation helps calm inflammation, set expectations, and start a stepwise plan that protects recovery.
Yes. Our priority is medical care and functional recovery. We coordinate with physical therapists, occupational therapists, and, when appropriate, employers or case managers to support return-to-work plans. If you retain an attorney, we provide objective documentation and communicate when appropriate. Collaboration ensures your treatment plan, restrictions, and milestones are aligned across your care team for consistency and progress.
Bring any imaging and reports if available, a list of medications and allergies, a timeline of your injury and symptoms, and details about job or sport demands. Wear comfortable clothing for exam and movement testing. If you use braces or orthotics, bring them. Clear information helps us design a practical, right-sized plan that addresses your goals and daily realities.
It’s common for pain to emerge hours or days later as inflammation increases and muscles tighten. Delayed symptoms don’t make your injury less real. Seek evaluation if pain interferes with work, sleep, or activity; if numbness, tingling, or weakness develops; or if headaches, dizziness, or visual changes follow impact. Early guidance reduces setbacks and supports a safer, predictable recovery trajectory.
Contact us and set up your doctor visit today to start your journey to pain-free living