Foraminal stenosis and spinal stenosis are two conditions that cause narrowing of the spinal canal. Both conditions can cause pain and weakness, but there are some differences between them. In this short blog, we’ll explore the different causes, symptoms, and treatment options for both foraminal stenosis and spinal stenosis. We will also discuss how to differentiate between the two conditions so that you can make an informed decision about the best course of action for your particular situation.
What’s the Difference Between Foraminal Stenosis and Spinal Stenosis?
Spinal stenosis is the narrowing of one or more spaces of your spine. This reduces the amount of room available for both your spinal cord and the nerves that run off it, causing them to become irritated, compressed, or pinched. While Spinal Stenosis usually develops slowly over time, it can lead to back pain and sciatica, which can cause serious leg weakness or bowel or bladder changes.
Foraminal Stenosis is actually a type of Spinal Stenosis, where the openings (“foramen”) between the bones in your spine narrow or tighten. Like Spinal Stenosis, this too can cause the nerve roots passing through your spinal cord to get pinched. This can cause pain, numbness, and weakness in the part of the body the nerve serves, as well as radiating pain that extends to other parts of the body.
What Causes These Conditions?
Spinal stenosis usually develops slowly over time, and is most often caused by “wear-and-tear” changes (such as osteoarthritis) that naturally occur as you age. This is why many people don’t experience symptoms right away, and can often go a long time without experiencing pain or discomfort.
Foraminal Stenosis is also caused primarily by age, as well as age-related symptoms. For example, arthritis can often cause changes in your spine over time, which can cause the foramen, or “openings in your spine” to narrow. Foraminal stenosis can also be caused by a bulging or herniated disk, which can press on the foramen and the nerve root, usually in your lower back.
Bone spurs (smooth, bony lumps that grow off a bone) can also cause both types of stenosis, as they can often pinch the nerves running through and around your foramen. Other less common causes of stenosis include thickened ligaments, spinal fractures, spinal cord cysts or tumors, and congenital spinal stenosis, a condition in which a person is born with an abnormally small spinal canal.
Can I Prevent Spinal or Foraminal Stenosis?
While you can’t necessarily prevent stenosis, staying physically active and maintaining a healthy weight can help reduce your risk. Moreover, taking steps to prevent back injuries which can lead to stenosis can also help lower your risk. That’s why maintaining a good posture and using proper form when lifting heavy objects is important.
Symptoms of Spinal and Foraminal Stenosis
While many people don’t experience any symptoms of foraminal stenosis, they can experience pain and discomfort if their nerves are moderately compressed. Symptoms of foraminal stenosis include local pain, numbness, weakness, and sensations of burning or tingling in the extremities affected. Traveling pain ‘along the nerve’s path’ is also common.
Spinal stenosis may affect any part of the spine but is more prevalent in the lumbar, or “lower back.” Lumbar spinal stenosis usually produces pain in the buttocks, thighs, and calves when walking or standing, whereas cervical spinal stenosis can affect the body from the neck down.
While not everyone will experience severe pain, weakness, or numbness, ignoring stenosis can cause your nerves to die, resulting in a loss of function. This can cause you to lose the ability to feel sensations in your extremities.
Treatment Options for Spinal & Foraminal Stenosis
Many of the symptoms of both spinal and Foraminal stenosis can be managed with nonsurgical treatments—including pain medication and low-impact exercises, among other options. That said, if nonsurgical treatments are unsuccessful in relieving your symptoms, surgery may be recommended, which can help enlarge the size of the spaces of your spine, helping to relieve the nerve compression.
Get Treatment for Spinal Stenosis in Dallas
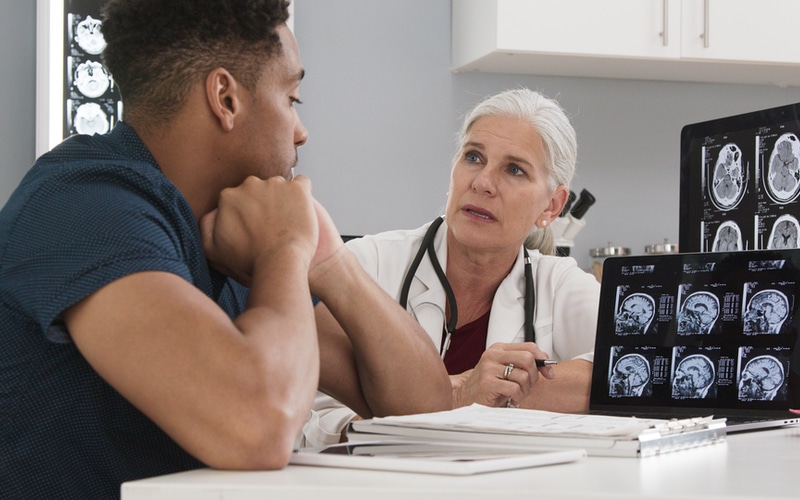
Are you experiencing pain or discomfort in your lower back or neck, or feeling numbness or weakness in your extremities? Both spinal and foraminal stenosis can be debilitating conditions that can progressively worsen over time. That’s why it’s important to see a specialist as soon as possible if you’re experiencing pain or discomfort of any kind.
If you need either foraminal stenosis or spinal stenosis treatment in Dallas, contact our office to schedule an appointment. We’ll perform a thorough diagnosis of your condition and provide the treatment you need to experience lasting relief.